Resources
Findings: In this cohort study of 1020 adults that used a combined instrumental variable analysis and matching approach, participation in a medically ...
Learn More
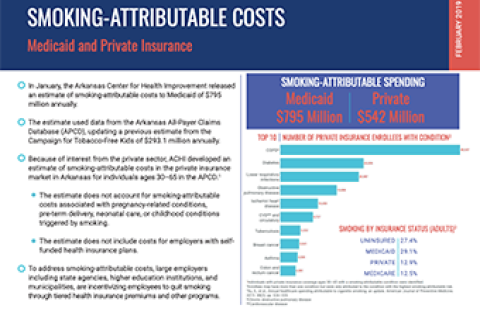
To estimate the cost of smoking to Medicaid, ACHI analyzed data from the Arkansas All-Payer Claims Database to determine the amounts of claims paid by...
Learn More
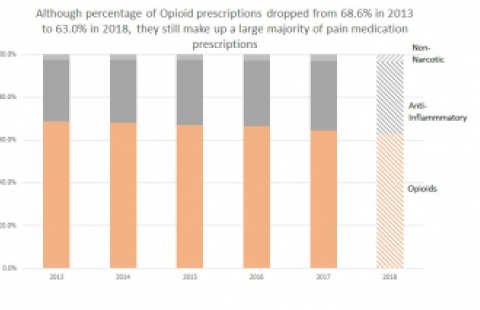
This DataByte looks at both the percentage of opioid prescriptions and length of days supplied. The data for these results comes from the Utah All Pay...
Learn More
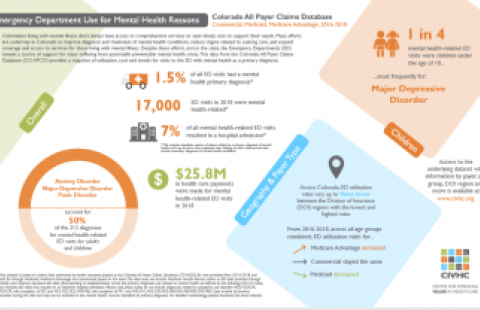
The Emergency Department (ED) Mental Health-Related report provides stakeholders the opportunity to compare utilization and cost metrics for ED visits...
Learn More
This resource details all use cases produced using Minnesota claims as of October 2017.
Learn More
The Minnesota Department of Health, Health Economics Program, using 2012 and 2015 data from the MN APCD, produced a brief looking at the rates of opio...
Learn More
Minnesota's State Health Access Data Assistance Center (SHADAC) evaluated the success of the State Innovation Model (SIM) initiative from 2015-20...
Learn More
The Minnesota Department of Health used Minnesota claims data from 2012 to analyze administrative healthcare transactions for 4.3 million privately an...
Learn More
The Minnesota Department of Health utilized claims data from the Minnesota All-Payer Claims Database (MNAPCD) to analyze pharmaceutical spending and u...
Learn More
The Minnesota Department of Health analyzed the overuse of unnecessary or low-value care throughout the state of Minnesota using data from the MN APCD...
Learn More
This report examines chronic disease prevalence and spending for Minnesota residents with health insurance in 2012, using Minnesota’s robust All Payer...
Learn More
A research study that measures special care days (SCDs) (intermediate or intensive), length of stay, and readmission rates among low-risk neonates acr...
Learn More
In this DataByte, Utah’s All Payer Claim Database (APCD) 2020 vaccination data trend is compared with the 2019 vaccination data trend[1]. The APCD con...
Learn More
The New England Public Policy Center at the Boston Fed recently released a report entitled “Medication-assisted Treatment for Opioid Use Disorder in R...
Learn More
Goal: Determine financial impact that an increase in reimbursement would have on the overall Medicaid budget and the number of Optometrists and access...
Learn More
Goal: Evaluate prior coverage analysis, de-identified and aggregated by payer, which depicts measures of data quantity (number of members, number of c...
Learn More
This research entity will define patterns of opioid analgesia and prolonged opioid use in a large cohort study of patients that underwent major inpati...
Learn More
A research study that measures special care days (SCDs) (intermediate or intensive), length of stay, and readmission rates among low-risk neonates acr...
Learn More
Washington State Office of Financial Management staff used the WA-APCD to run Pharmacy Quality Alliance Opioid Prescribing Measures for 2014-2018.
Learn More
This analysis helps to answer, of the people who have a fecal screener: 1. How many insured lives in Colorado have a colonoscopy within a year?, and, ...
Learn More